Cannabidiol is a safe, non-intoxicating, and non-addictive cannabis compound with significant therapeutic attributes, but CBD-drug interactions may be problematic in some cases. CBD can potentially interact with many pharmaceuticals by inhibiting the activity of cytochrome P450, a family of liver enzymes. This enzyme group metabolizes most of the drugs we use. At sufficient dosages, CBD will temporarily deactivate cytochrome P450 enzymes altering how we metabolize a wide range of compounds.
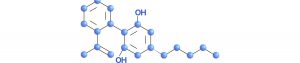
When a foreign compound enters the body, it is metabolized. These liver enzymes also metabolize CBD, converting it into 7-OH–CBD and 6-OH–CBD. Different routes of cannabinoid administration have different effects. Inhaled CBD enters capillaries in the lungs, passes into general circulation through the pulmonary arteries, and quickly crosses the blood-brain barrier. When ingested orally, however, CBD is absorbed in the small intestine and then carried to the liver, where it is metabolized.
Lester Bornheim, a research pharmacologist at the University of California in San Francisco, was among the first scientists to study the metabolism of CBD. CBD, of all the plant cannabinoids studied, is the strongest cytochrome P450 deactivator. In 1999, Bornheim addressed the annual gathering of the International Cannabinoid Research Society (ICRS) and drew attention to the possibility that CBD could interfere with the metabolism of many medications. A year earlier, a team of Canadian scientists identified certain compounds in grapefruit that inhibit the expression of some cytochrome P450 enzymes—which is why physicians often warn patients not to eat grapefruit before taking their meds.
Bottom line: A person taking a CBD-rich product should pay close attention to changes in blood levels and adjust dosage accordingly and under the advice of a medical professional. For more information, visit Project CBD
Follow us on Twitter @bchsidemed Instagram @beachsidemedicalcbd